The Role of Prescription Monitoring Programs in Protecting Your License
Doug Jorgensen
May 11, 2025
If you prescribe controlled substances—opioids, benzodiazepines, stimulants—you already know your license is under more scrutiny than ever. The days of casual refills without a full chart review are gone. Regulators expect you to prove that you’re not just prescribing responsibly—you’re actively monitoring for misuse, diversion, and overprescribing patterns.
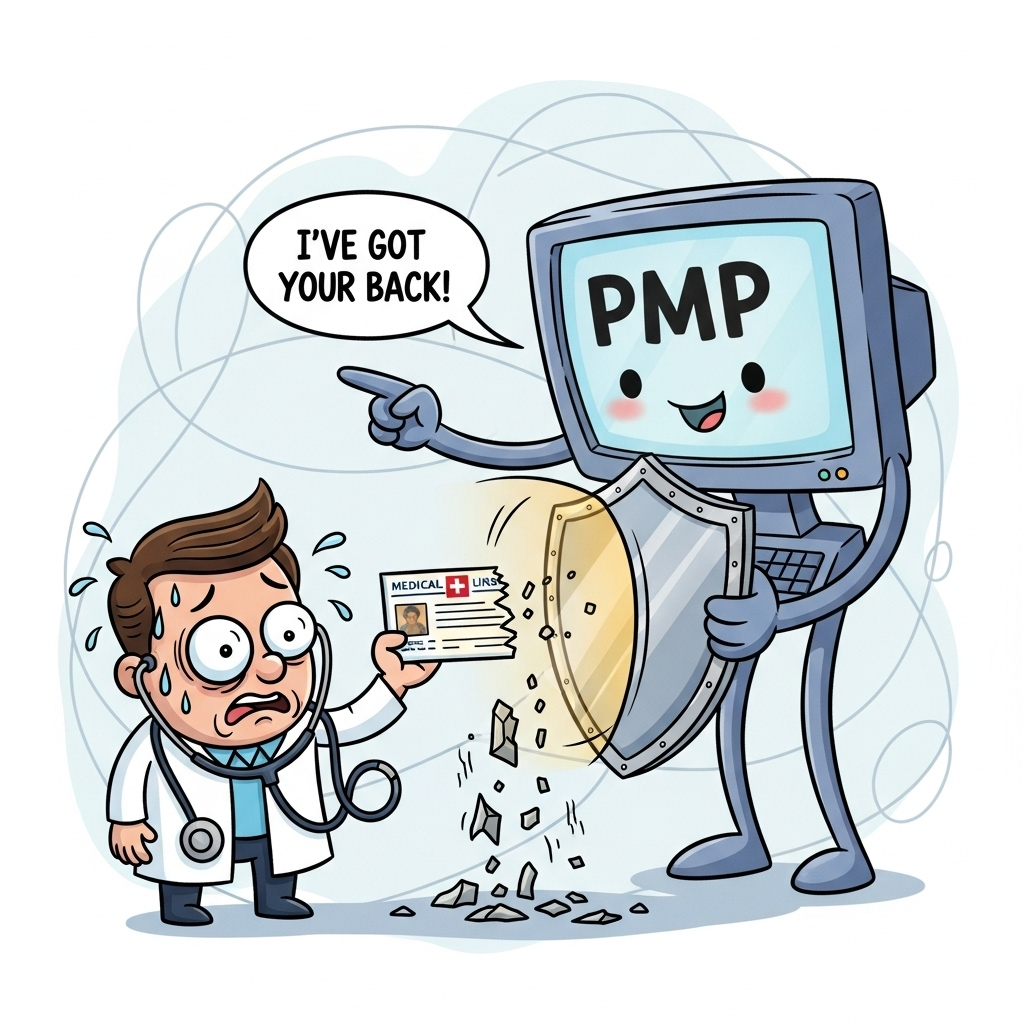
One of the most powerful tools we have for that is the Prescription Monitoring Program (PMP). And yet, I still see providers treating PMP checks like optional homework. That’s a mistake—one that can cost you your license.
What a PMP Actually Does
A Prescription Monitoring Program is a secure, state-run database that tracks controlled substance prescriptions dispensed by pharmacies. It allows you to:
- See every controlled substance a patient has received in a given timeframe.
- Identify multiple prescribers or overlapping prescriptions.
- Spot “pharmacy shopping” patterns.
- Verify that your prescribing matches the patient’s documented treatment plan.
Why PMP Checks Are a Compliance Shield
From a regulatory standpoint, if you prescribe without checking the PMP, you’re essentially flying blind. In the event of:
- A state board complaint
- A DEA audit
- A malpractice claim
…the first question is often, “Did you check the PMP?” If the answer is “no,” you’ve already lost ground—because the expectation is that you will, every time, for every controlled prescription.
When to Use the PMP
I recommend—and in many states, it’s required—that you check the PMP:
- At every initial controlled substance prescription.
- At every refill.
- When patients request an early refill.
- When new concerning behaviors arise (lost prescriptions, missed appointments, etc.).
How PMP Data Protects You
Let’s say a patient comes in requesting an opioid refill. You check the PMP and see they’ve recently filled the same prescription from another provider. Now you have a defensible reason to pause, investigate, and document. Without that PMP check, you could have unwittingly contributed to diversion—and your chart note would not protect you.
Best Practices for PMP Use
- Document the Check – Include the date and any relevant findings in your note.
- Discuss Concerns with the Patient – Address discrepancies directly, and record the conversation.
- Integrate into Workflow – Assign a staff member to run PMP reports before you see the patient so you have the data in-hand.
A Quick Story
I once consulted for a clinic under investigation after a patient’s overdose. The lead provider had a strong chart—good history, physical, and plan—but had not documented any PMP checks. Investigators assumed no checks were done–this was not the case. That assumption was a key factor in their disciplinary action as it became very hard to prove he was using the PMP. Documentation is your proof—without it, it’s as if the PMP check never happened.
Bottom Line
The PMP is more than a compliance box to check—it’s your early warning system and one of the most powerful tools you have to protect both patients and your license.
If it’s not in the PMP, you don’t know the whole story. And if it’s not documented, it didn’t happen.
About the Author
Douglas J. Jorgensen, DO, CPC, FAAO, FACOFP
Dr. Doug is a physician, consultant, and national educator on medical documentation accuracy, patient engagement, and compliance strategy. He helps healthcare organizations develop systems that make patients active partners in their own medical records.