Why the US Healthcare System Struggles With Universal Coverage
Doug Jorgensen
March 9, 2025
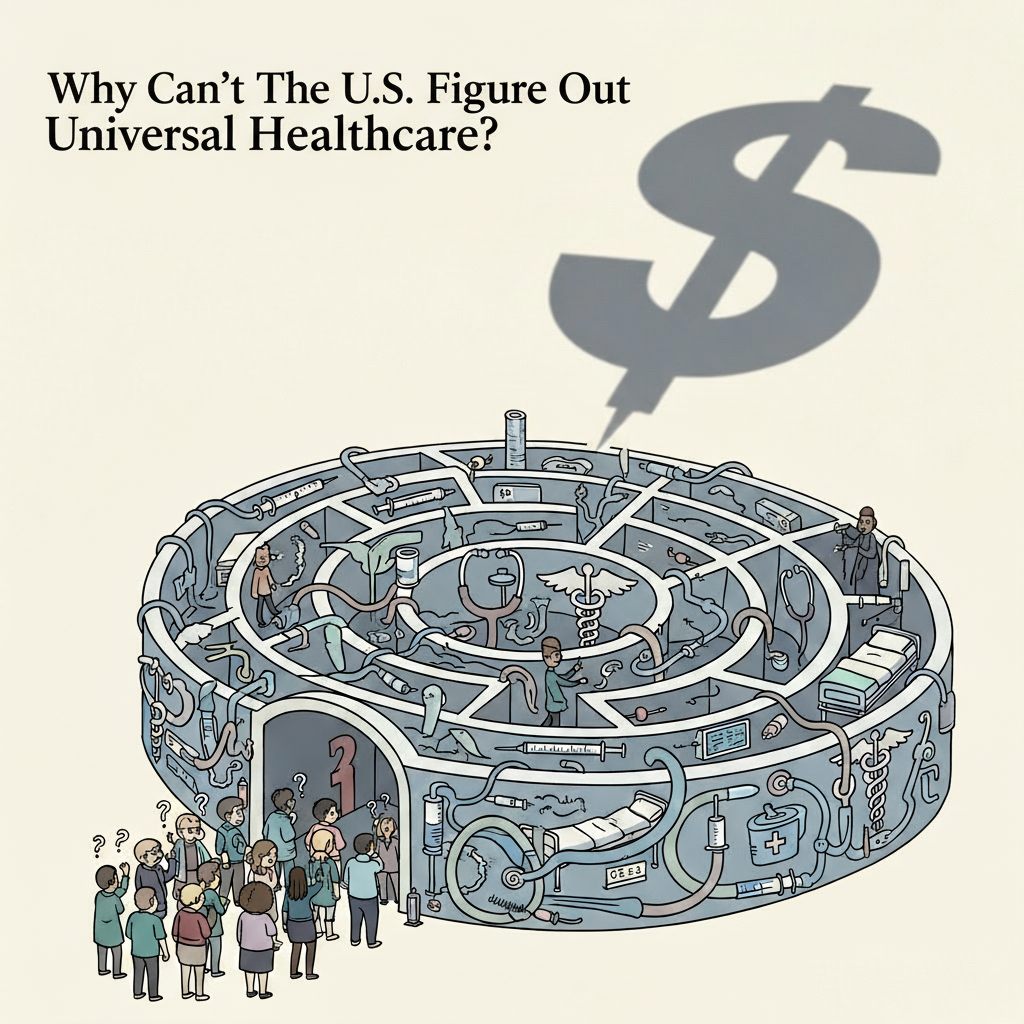
Introduction: A System Built for Something Else
The United States has some of the most advanced medical technology, highly trained specialists, and cutting-edge research in the world.
So why is universal healthcare coverage such a challenge here—when dozens of other developed nations have managed it?
The short answer: the US healthcare system wasn’t designed for universal coverage in the first place.
The Original Purpose: Catastrophic Care
American health insurance began as a way to protect patients from catastrophic medical costs, not to cover every aspect of healthcare.
- In the early 20th century, most care was paid out-of-pocket.
- Employer-sponsored health insurance expanded during WWII as a workaround for wage freezes.
- Medicare and Medicaid were introduced in 1965 to protect the elderly, disabled, and low-income populations.
The result? A patchwork system that left large gaps—especially for preventive and primary care.
A Culture of Employment-Based Coverage
Unlike countries where health coverage is a citizenship right, the US tied health insurance to employment:
- Large employers negotiated private plans.
- Those outside the workforce often relied on public programs—or went uninsured.
- Job changes, layoffs, or self-employment could mean losing coverage entirely.
This structure makes expanding to universal coverage complex, because it would require replacing or integrating millions of existing private plans.
The Role of Private Insurance
Private insurers are deeply embedded in the US system:
- They manage most employer-sponsored plans.
- They administer many Medicare Advantage and Medicaid managed care programs.
- They wield significant lobbying power, influencing policy design.
Any move toward universal coverage must account for (or overcome) the economic and political weight of these companies.
Cost Structure Challenges
The US spends more per capita on healthcare than any other nation, yet outcomes don’t always match that investment. High costs come from:
- Administrative overhead in a multi-payer system
- Higher prices for drugs and procedures
- Defensive medicine driven by litigation fears
- Expensive infrastructure and technology adoption
Universal coverage in a system with these cost drivers would require either major cost control reforms or significantly higher funding.
Political Polarization
Healthcare reform in the US is politically charged:
- Universal coverage proposals are often labeled as “socialized medicine.”
- Voter support is split along ideological lines.
- Legislative efforts face intense lobbying from insurers, pharmaceutical companies, and provider groups.
This polarization makes comprehensive reform slow and contentious.
Lessons from Other Countries
Countries with universal systems built them on:
- Broad-based taxation from the start
- Strong primary care foundations
- Public buy-in for collective responsibility over healthcare costs
The US lacks these starting conditions, making retrofitting universal coverage far more complex. Not impossible but hard questions must be asked and answered. Achieving consensus will be difficult..
Moving Forward
If the US wants to move toward universal coverage, key steps could include:
- Cost Containment – Reducing administrative waste and negotiating lower drug prices.
- Primary Care Strengthening – Investing in preventive services to reduce long-term costs.
- Hybrid Models – Maintaining private insurance options alongside a public baseline plan.
- Phased Rollout – Starting with expanded eligibility for Medicare or Medicaid.
Final Thoughts: The System We Built
The US doesn’t struggle with universal coverage because it’s impossible—it struggles because our system was built for a different purpose and has evolved around that original design. Additionally, the healthcare system, originally established over 60 years ago, is struggling to cope with current funding requirements and modern medical demands due to population growth and increased life expectancy.
You can retrofit an old house to meet modern needs, but it takes time, money, and a willingness to tear down walls.
About the Author
Douglas J. Jorgensen, DO, CPC, FAAO, FACOFP
Dr. Doug is a physician, consultant, and national educator on healthcare policy and regulatory compliance. He brings historical and policy perspective to debates about healthcare reform in the United States.