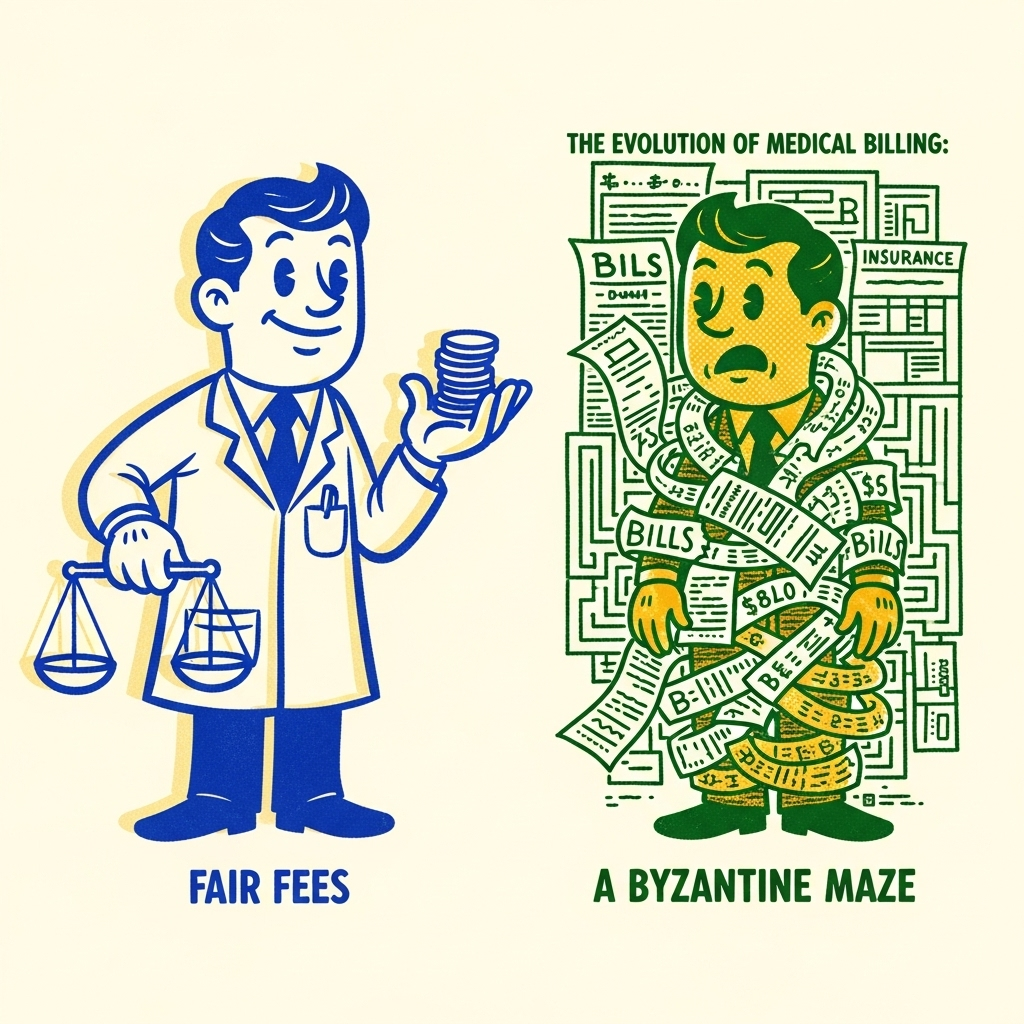
The Evolution of Medical Billing: From Fair Fees to a Byzantine Maze
Doug Jorgensen
February 25, 2025
Introduction: When “Reasonable and Customary” Actually Meant Something
There was a time—not that long ago—when medical billing was straightforward.
You provided a service, charged a reasonable fee, and the insurer paid a fair share based on what other providers in your area charged for the same service.
It was called “reasonable and customary” billing. It wasn’t perfect, but it was predictable.
Then came the shift—a move away from fairness and toward complexity, control, and opacity.
Today’s billing system isn’t just confusing—it’s a carefully engineered labyrinth designed to advantage insurers, not patients or providers.
The Old Model: Reasonable and Customary
- How It Worked:
Insurers surveyed local billing data to determine the going rate for each service.
Providers set their fees accordingly, knowing they’d be fairly reimbursed. - Advantages:
- Regional cost differences were respected.
- Providers could focus on care instead of coding gymnastics.
- Patients had fewer surprise bills.
- Regional cost differences were respected.
The Shift: Enter Medicare-Based Fee Schedules
In the 1990s, insurers began using Medicare fee schedules as the baseline for reimbursement—not because it was more accurate, but because it was cheaper.
- Medicare rates were originally designed for government programs, not private insurance.
- Private insurers began applying these rates across the board, often paying just 110–130% of the Medicare rate, regardless of actual market value.
The result?
- Urban and rural cost differences disappeared.
- Practices with higher overhead (like rural clinics) got squeezed.
- Patients saw network narrowing as providers opted out.
Layering on Complexity: The CPT and ICD Code Explosion
As the system evolved:
- CPT (procedure) codes multiplied.
- ICD (diagnosis) codes became increasingly granular.
- New “modifier” codes were added to capture nuances—and often to justify payment for work already done.
On paper, it looked like precision.
In reality, it created an administrative arms race where billing specialists had to outmaneuver insurance algorithms just to get paid.
Why It’s Now a Byzantine Maze
Today’s billing process is:
- Opaque – Patients rarely know the cost until after the service.
- Inconsistent – The same procedure can be reimbursed at wildly different rates depending on contracts.
- Exploitable – Insurers use complexity to delay, deny, or reduce payments.
And here’s the kicker: many denials are reversed if appealed—because the initial “no” was more about attrition than accuracy.
Impact on Providers
- Lower Margins – Less revenue for the same work.
- Higher Overhead – More staff and software to manage billing.
- Burnout – Providers spending more time on coding and compliance than patient care.
Impact on Patients
- Surprise Bills – Out-of-network trapdoors hidden in “covered” services.
- Access Issues – Fewer providers willing to accept certain plans.
- Higher Costs – As administrative bloat gets passed along in premiums and deductibles.
Can It Be Fixed?
Not without confronting the root problem: the misalignment of incentives.
Right now:
- Insurers profit from complexity and reduced payouts.
- Providers lose time and money fighting for fair reimbursement.
- Patients shoulder the ultimate financial and health consequences.
Final Thoughts: The Need for a Return to Clarity
We can debate fee schedules and coding systems all day, but the truth is simple:
A transparent, regionally adjusted reimbursement system—one that rewards efficiency without penalizing good care—would benefit everyone except those profiting from the current mess.
Until then, providers must navigate the maze with vigilance, document relentlessly, and educate patients about the forces at work behind every bill they receive.
About the Author
Douglas J. Jorgensen, DO, CPC, FAAO, FACOFP
Dr. Doug is a physician, consultant, and national educator on healthcare policy and regulatory compliance. He specializes in helping providers navigate the financial and administrative realities of modern medicine.


