The Truth About Entitlement Programs: What Medicare and Medicaid Actually Do
Doug Jorgensen
February 13, 2025
Introduction: “Entitlement” Isn’t a Dirty Word—It’s a Legal One
In today’s political climate, few terms get tossed around with more heat and less understanding than “entitlement programs.”
You’ve heard the commentary:
“People just want handouts.”
“These programs are bankrupting the system.”
“Medicare and Medicaid are bloated and broken.”
But take a step back. Strip away the soundbites and headlines. What are entitlement programs actually? Who gets them, how do they work, and why were they created in the first place?
As a physician who’s worked inside this system for decades—and testified in front of federal regulatory bodies—I can tell you with confidence: Most Americans don’t know how these programs function or why they exist.
So let’s fix that.
What Is an Entitlement Program?
Let’s define it properly:
An entitlement program is a government program that provides benefits to individuals who meet certain eligibility criteria, regardless of the program’s budget status.
That’s it.
You’re entitled to benefits because you meet the qualifications—whether that’s based on age (Medicare), income (Medicaid), disability, or work history (Social Security).
These are not giveaways. They are legally earned or need-based rights, backed by law.
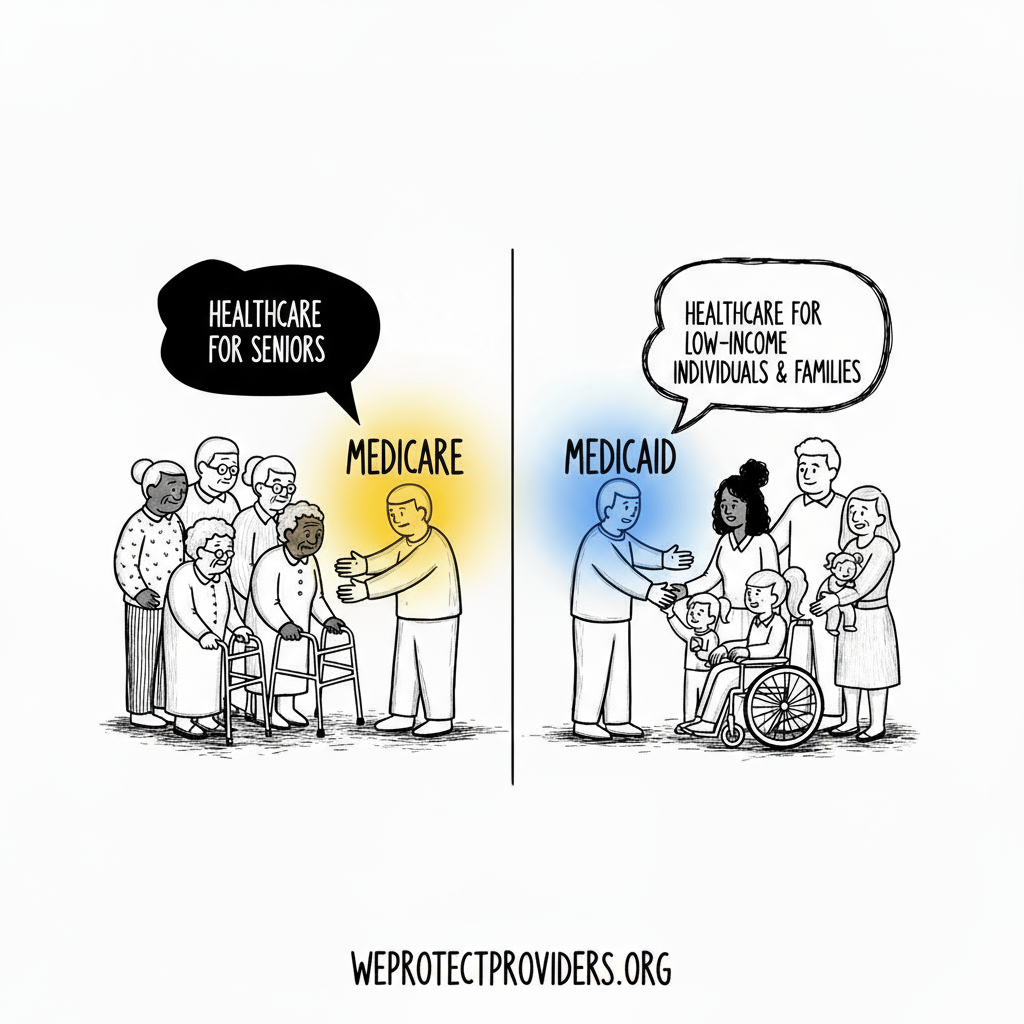
A Quick Breakdown: Medicare vs. Medicaid
Though often lumped together, Medicare and Medicaid are two very different programs:
Medicare
- A federal program
- For people 65 and older or with qualifying disabilities
- Funded by payroll taxes (you pay into it during your working years)
- Administered by CMS (Centers for Medicare & Medicaid Services)
Medicaid
- A joint federal and state program
- For individuals and families with low income and limited resources
- Funded by both federal and state governments
- Administered at the state level (so it varies by location)
These programs are often the only safety net available for the elderly, disabled, and poor. They don’t overlap often, but when they do, the individual is known as “dual eligible.”
So Why the Bad Reputation?
Two reasons:
1. Political Language
The term “entitlement” has become shorthand for “something for nothing.” It’s been used as a weapon in budget debates, campaign rhetoric, and media cycles.
But the truth is:
If you’ve paid into Medicare, you’ve earned it.
If you qualify for Medicaid, you’ve passed strict means testing.
This isn’t freeloading—it’s policy working as designed.
2. Frustration With the System
It’s true: these programs have problems.
- Long wait times
- Confusing billing
- Limited coverage
- Reimbursement challenges for providers
But that’s not because they’re “entitlement” programs. It’s because they were built decades ago, expanded without redesign, and left to operate in a rapidly evolving healthcare landscape.
How These Programs Actually Function
Here’s what most people don’t realize:
➤ Medicare and Medicaid aren’t healthcare systems. They’re payment systems.
They don’t treat patients. They fund the treatment.
➤ They operate within narrow rules.
Coverage is limited to what’s considered “reasonable and necessary” based on federal criteria. If your service, test, or drug falls outside that? You pay—or go without.
➤ They are administered by CMS from Baltimore, Maryland.
The same central agency governs both programs. And their job is less about care—and more about compliance, documentation, and cost control.
Federal vs. State: A Hidden Divide
While Medicare is standardized nationally, Medicaid is anything but.
Each state:
- Sets its own eligibility rules
- Defines its own covered services
- Negotiates provider payment rates
- Manages its own administrative structure
That’s why a Medicaid patient in New York might have access to dental coverage and vision services—while someone in Texas may not.
This leads to a fragmented experience for patients, even though they’re all part of a so-called national entitlement system.
Entitlements in Practice: A Few Myths Debunked
Myth 1: These programs are bankrupting America.
Reality: While costs are high, they are in line with population needs. The real inefficiencies lie in administrative complexity and profit-driven private plans, not the programs themselves.
Myth 2: People abuse the system.
Reality: Fraud exists—but it’s a small fraction of total spending. The majority of patients use these programs responsibly, often as their only option.
Myth 3: Providers love government programs.
Reality: Many providers lose money seeing Medicaid patients due to low reimbursement. That’s not a flaw of entitlement—it’s a failure of payment policy.
Why Understanding This Matters—For Patients and Providers
If you’re a patient, this knowledge helps you:
- Understand your rights
- Advocate for your care
- Anticipate what’s covered (and what’s not)
- Recognize when to seek supplemental coverage
If you’re a provider, it helps you:
- Set realistic expectations with patients
- Navigate reimbursement and documentation challenges
- Understand federal and state compliance differences
- Engage more effectively in policy discussions
Closing Thoughts: These Programs Aren’t Perfect—But They’re Necessary
The truth about Medicare and Medicaid is complicated—but essential.
They were born out of real public health needs. They’ve evolved under the weight of budget pressures, population shifts, and politics. And while they’re imperfect, they remain the foundation of healthcare access for millions.
Let’s stop demonizing the word “entitlement” and start understanding it.
Let’s fix what’s broken—but preserve what works.
And above all, let’s remember: Healthcare isn’t a luxury. It’s a responsibility we share—especially for those who can’t fight for themselves.
About the Author
Douglas J. Jorgensen, DO, CPC, FAAO, FACOFP
Dr. Doug is a physician, medical policy advisor, and federal consultant with decades of experience inside Medicare, Medicaid, and healthcare regulation. He works at the intersection of patient care and healthcare finance, advocating for clarity, accountability, and smarter policy.