Introduction: The False Comfort of Routine Prescribing
Let me be blunt: If you’re prescribing controlled substances without a structured risk mitigation plan, you’re playing a dangerous game—both for your license and your patients.
Far too many providers—especially in primary care and psychiatry—treat benzodiazepines, amphetamines, and even low-dose opioids as if they’re benign. “I trust my patients,” they say. Or, “We only give it to a few people.” I’ve heard every version of that rationale during my years reviewing medical records for litigation, audits, and federal investigations.
Here’s the truth: Trust without verification is not a compliance strategy. It’s a liability.
If you prescribe controlled substances, there are five non-negotiables you must have in place. These aren’t suggestions. They’re the regulatory seatbelt that keeps you from flying through the windshield when a government agency, payer, or disgruntled patient hits the brakes.
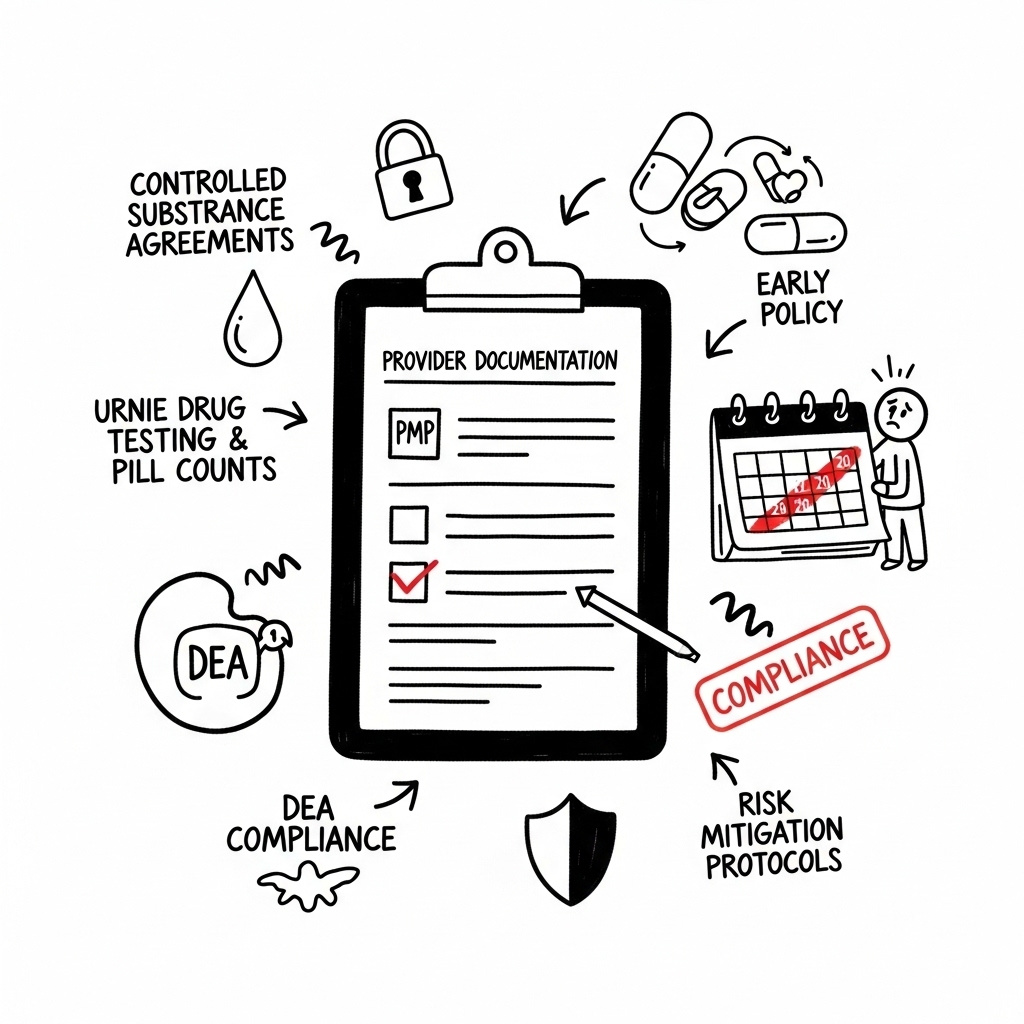
1. Prescription Monitoring Program (PMP) Checks—Every. Single. Time.
I don’t care if it’s the patient’s tenth refill, if they “seem fine,” or if you’re busy and running behind.
You must run a PMP check before every controlled substance prescription is written. Why?
- It confirms no other providers are prescribing duplicate or conflicting medications.
- It catches early signs of shopping or diversion.
- It provides a verifiable timestamp that you are engaged in due diligence.
This step takes 30 seconds and can save your license. Skipping it is indefensible in an audit.
2. Controlled Substance Agreements (CSAs)
A controlled substance agreement isn’t just paperwork—it’s legal insulation. It defines expectations and gives you the leverage to say “no” without ambiguity. It is not a contract, as contract implies an obligation by both parties; in this case you to prescribe for your patient. In a CSA the provider is in the driver’s seat.
Key elements should include:
- A single prescriber policy
- Prohibited behaviors (early refills, sharing meds, mixing with alcohol)
- Mandated and random pill counts and urine testing
- Consent to PMP checks
- Probation and eventually Termination policy for violations
If you’re prescribing without one of these in place, you’re putting all the risk on your shoulders—and your malpractice carrier may not cover you when it goes sideways–they only cover civil matters, not criminal.
3. Urine Drug Testing (UDT) on a Schedule—Not Just When It Feels Suspicious
A UDT policy must be proactive, not reactive.
Here’s the minimum cadence I recommend:
- Quarterly for chronic users of any Schedule II or III drug
- Every other month for moderate to high-risk patients
- Random testing if any inconsistencies, red flags, or behavioral shifts occur or–and this is strongly advised–use a randomizer so you are not playing favorites with your patients.
UDT isn’t about catching liars or playing ‘gotcha’—it’s about validating responsible prescribing. It gives you data, it documents safety, and it becomes your first line of defense when an inquiry arises.
Pro tip: Always confirm results with mass spectrometry when needed. Screening-only testing doesn’t hold up under legal scrutiny.
4. Pill Counts: Documented and Random
Pill counts are one of the most underutilized and powerful tools available.
Here’s how they work:
- You notify the patient randomly to bring in their medication.
- You compare what they should have vs. what they do have.
- You document the result.
If they’re short, it may be a sign of misuse or diversion. If they’re over, it may indicate non-compliance.
Either way, you now have objective data that informs your clinical decisions—and protects you in court.
5. Tracking Early Refills and “Lost” Medications
If you’ve been in practice long enough, you’ve heard it all:
- “I spilled it down the sink.”
- “My dog ate it.”
- “The pharmacy shorted me.”
- “I just need five more to get me through the weekend.”
None of these are good enough. Every early refill request or claim of lost medication must be:
- Logged in the patient’s chart
- Documented with your rationale
- Counted toward policy violations outlined in the CSA
The pattern is the point. These seemingly small requests build a profile—one that federal investigators know how to follow.
Why This Matters More Than Ever
The regulatory environment isn’t softening—it’s hardening.
Government oversight of controlled substance prescribing has expanded beyond opioids to include:
- Benzodiazepines (e.g., Xanax, Ativan)
- Amphetamines (e.g., Adderall, Vyvanse)
- Antiseizure Agents (gabapentin and pregabalin)
- Buprenorphine and even testosterone in some cases
If you don’t have risk mitigation protocols in place, you’re exposed. It’s not fear-mongering. It’s experience. I’ve been in the room with investigators, prosecutors, licensing boards, and payers. I’ve seen good clinicians suffer avoidable consequences because they didn’t have systems in place.
Final Thoughts: Don’t Be the Outlier Without a Defense
Being a statistical outlier isn’t necessarily a bad thing—if your care is excellent and your documentation is airtight. But if you’re an outlier with no risk mitigation? You’re just a headline waiting to happen.
These five tools aren’t hard to implement. They aren’t expensive. And they aren’t just about compliance—they’re about professionalism, responsibility, and respect for the power of the medications we prescribe.
You can’t control what the government will do next. But you can control how prepared you are when they show up.
About the Author
Douglas J. Jorgensen, DO, CPC, FAAO, FACOFP
Dr. Doug is a nationally recognized regulatory consultant, expert witness, and federal policy advisor specializing in controlled substance prescribing, medical audit defense, and healthcare compliance. He has conducted over 100,000 medical record audits and served as an expert for DOJ, DEA, CMS, and OIG.